Introduction
In the world of healthcare, we’re seeing some pretty big changes thanks to artificial intelligence (AI). One key area where AI is really making a difference is in managing chronic pain. A lot of people around the globe suffer from chronic pain, which creates huge challenges not just for them personally but also economically. The usual ways of dealing with pain don’t always work well for everyone. But now, AI is stepping in and offering new hope.
With tools like predictive diagnostics, natural language processing, and even robotics powered by AI are changing how doctors approach pain management. These tech advancements mean that diagnosing problems can be more accurate than ever before; they help keep patients involved in their own care and make sure treatments are tailored specifically to what each person needs. This move towards using AI in health stuff looks really promising for helping folks deal with chronic pain better.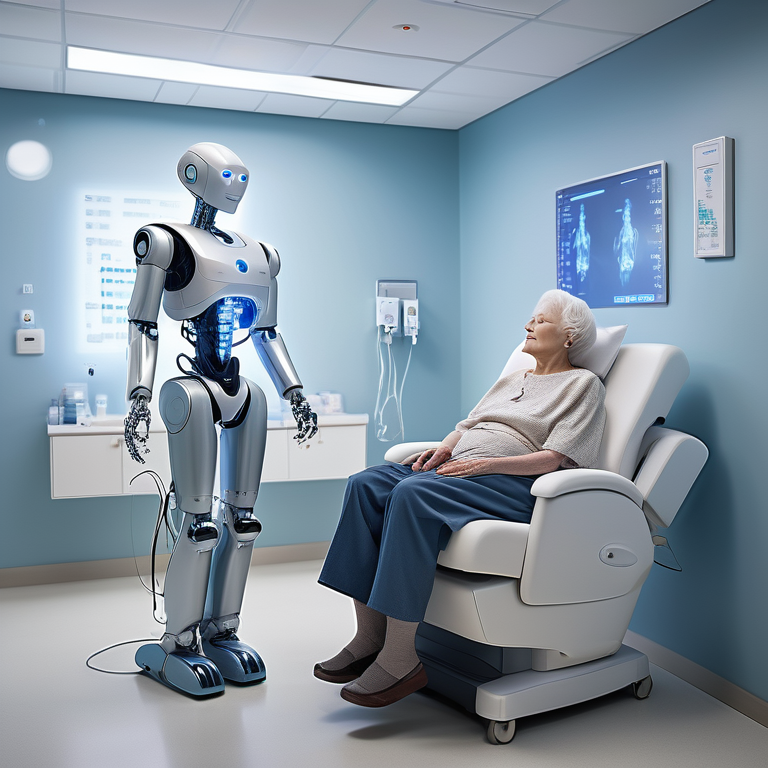
The Evolution of AI in Healthcare
In the healthcare world, artificial intelligence has really changed things up. With stuff like generative AI and neural networks leading the charge, we’re seeing some cool new tech in medicine. This means doctors can figure out what’s wrong with you more accurately, come up with better ways to treat you, and overall take care of patients better. By feeding these AI systems a ton of information, they get smarter over time. This is especially good news for folks dealing with chronic pain because it’s helping find better ways to manage it.
The beginning of AI in medicine
The journey of AI in healthcare started when people working on computer science and deep learning saw how it could change the way we treat illnesses. They created computer programs that could go through a lot of information quickly, making it easier to figure out what’s wrong with someone and how to treat them. By using deep learning, which involves complex artificial neural networks, the power of ai systems got even better for medical use. This was really the start of using AI in medicine, paving the way for today’s progress in managing long-lasting pain.
Current advancements in AI for healthcare
Right now, AI is making a big difference in many areas of healthcare, like helping people who suffer from long-term pain. By using machine learning, computers can look through huge amounts of data to help come up with treatment plans that are tailored just for them. Deep neural networks, which are really good at dealing with complicated information, play a key role in pushing forward the use of AI in healthcare. With these technologies at work, doctors can better manage pain for their patients, leading to better health results and higher quality care overall.
Understanding Chronic Pain and Its Impact
Chronic pain is a big health problem that touches the lives of millions around the globe. It’s when you’re in pain for more than three months straight. With chronic pain, life can get pretty tough – it can make your quality of life worse, cut down on how much work you can do, and bump up what you spend on healthcare. Figuring out how to manage this kind of pain isn’t easy because everyone needs something different to help them feel better. By bringing AI technology into the picture for managing pain, there’s a chance to make treatment plans better suited for each person dealing with chronic pain and possibly improve their situation.
Definition and types of chronic pain
Chronic pain covers a bunch of different health issues and gets sorted by what causes it or where you feel it. You’ve got things like nerve pain, muscle and bone pain, and really bad headaches as some common kinds. Treating each kind needs its own plan. With the help of AI technology, figuring out which type of pain someone has becomes easier, leading to treatments that are more tailored to the individual. By looking at lots of data from different places, AI helps doctors make better choices in how they handle chronic for patients making their care better overall. On top of this using operations research can make sure resources are used in the best way possible so managing chronic doesn’t waste time or money.
The socio-economic impact of chronic pain
In places like the United States, chronic pain really takes a toll not just on people’s health but also hits hard economically. About 1 in every 5 people live with this kind of pain, leading to huge amounts of money spent on healthcare and even more lost because folks can’t work as much or at all. It’s not only about the bills for doctors and medicine; it affects whether someone can do their job, enjoy day-to-day life, or feel happy overall. By using AI technology to manage chronic pain better, doctors could make treatments more effective and lessen how much chronic pain costs everyone involved – from those suffering directly from it to society in general.
AI Technologies in Pain Management
AI technologies are changing the way we manage pain by making diagnosis, treatment planning, and how we engage with patients better. With AI algorithms, predictive diagnostics can look through patient data to spot patterns and guess how well treatments might work. Thanks to natural language processing, ai systems can make sense of what patients say in their reports which helps doctors come up with care plans that are just right for each person. Robotics is also playing a big role in physical therapy and rehab by offering precise help exactly where it’s needed. All these advancements mean people dealing with pain get better care and see improved results from their treatments.
Machine Learning for predictive diagnostics
In the world of pain management, machine learning is playing a big role in creating models that can guess how well different treatments might work. These models look at things like what’s happened to the patient before, their symptoms, and results from tests to find patterns and make predictions about what treatments could be best. With machine learning, doctors have a better shot at choosing the right treatment for each person. This way, they can come up with care plans that are tailored just for them, making it more likely for patients to get better faster and helping manage pain in smarter ways.
Natural Language Processing for patient reports
In the world of healthcare, especially when it comes to managing pain, natural language processing (NLP) is making a big difference. It’s being used to go through what patients say and help doctors and nurses understand them better. With NLP, all those notes in electronic health records or the symptoms patients talk about can be quickly looked into by computers. This way, healthcare workers can spot trends or important bits of information that might help come up with treatments that are just right for each person. By combining NLP with speech recognition technology, AI systems are stepping in to make conversations between people seeking care and their caregivers smoother. This not only makes things more efficient but also helps folks feel more involved in handling their pain.
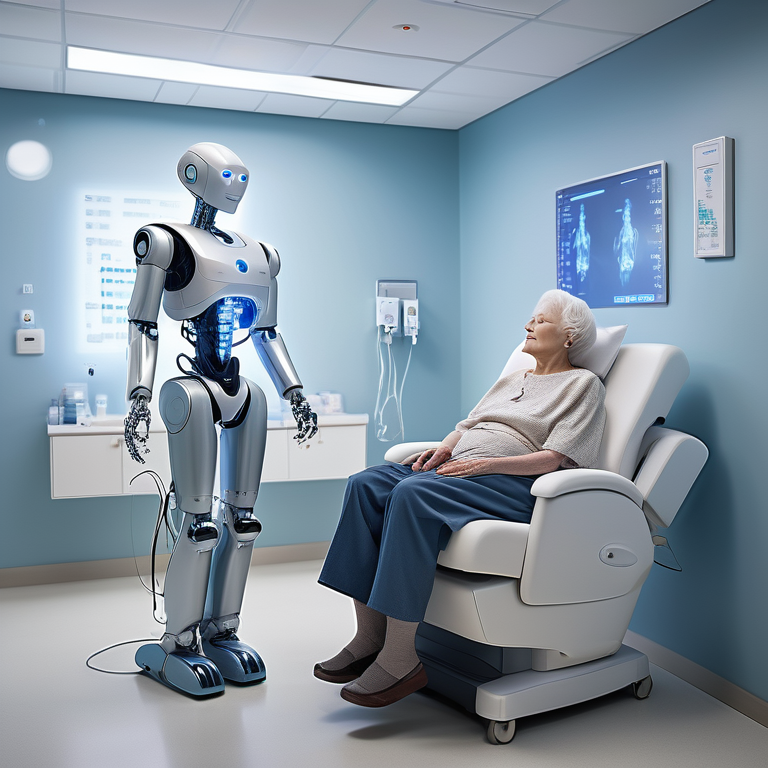
Robotics in Physical Therapy and Rehabilitation
In the world of pain management, robotics is making a huge difference in how physical therapy and rehabilitation are done. With the help of AI systems, these robots can offer very specific help that’s just right for what each person needs to feel better and recover faster. They’re smart enough to adjust their methods based on what works best for an individual patient, giving them a custom treatment plan. This blend of robotics with AI technology means doctors can make rehab programs much more effective at managing pain and helping patients get back on their feet quicker, all while boosting the quality of care they provide.
Case Studies: AI Success Stories in Chronic Pain Management
Through different examples, it’s clear that using AI in managing long-term pain works well. One area where AI shines is in precision medicine. Here, AI looks closely at each patient’s information to figure out the best treatment plan for them based on their specific traits. By using AI, doctors can create personalized treatment plans that really fit what each patient needs, making pain management better and patients happier. These examples show how powerful AI could be in changing how we handle chronic pain.
Implementing AI for Precision Medicine
In the world of healthcare, precision medicine is quickly changing how we approach treatment, making it more personal by looking at what makes each person unique. With a big focus on chronic pain management, AI is stepping up as a key player. It looks closely at heaps of information about patients – like their genes, past health issues, and how they’ve responded to treatments before – to figure out which treatment might work best for them. By bringing together big data and AI tools, doctors can now rely on solid facts to decide the best way to manage someone’s pain, leading to better results for patients.
Virtual reality as a pain management tool
Virtual reality, or VR for short, is starting to show a lot of promise in helping people manage pain. By putting patients into virtual worlds, it helps take their mind off the pain and gives them a feeling of calm and comfort. With VR, experiences can be customized based on what each person likes, making it more likely they’ll stick with it and find relief from their pain. On top of that, using VR might mean people don’t need to rely as much on strong painkillers that come with heavy side effects. As this technology gets better over time, we’re looking at VR playing a big role in making life easier for folks dealing with long-term pain.
Challenges and Considerations
AI technologies in healthcare show a lot of promise for making chronic pain management better. But, there are some big hurdles and things to think about. When it comes to using AI for health, we’ve got to be really careful about ethical issues. This includes worrying about bias and the moral questions that come up with artificial general intelligence. On top of that, keeping patient information safe is super important, so data privacy and security have to be strong. It’s also crucial to make sure there’s no gap between what AI can do and how doctors actually use it in their work. We need to ensure healthcare professionals know enough and have the right skills to use AI technologies well.
Ethical concerns in using AI for health
When we talk about using AI in healthcare, there are some big ethical questions that pop up and really need our attention. For starters, there’s a worry that AI might not treat everyone the same because of bias in its programming. This could mean unfair health outcomes for certain groups of people. To avoid this, it’s super important to make sure these ai systems learn from data that reflects all kinds of different folks.
Then there’s something called artificial general intelligence – basically when AI gets as smart as humans. We’ve got to think hard about what this means for who’s responsible when things go wrong, how clear they are about what they’re doing, and whether we might end up losing control over these technologies.
As ai systems keep getting better and smarter, making sure we have strong ethical rules is key so everything goes smoothly in healthcare.
Data privacy and security
When it comes to using AI for managing chronic pain in healthcare, keeping patient data safe and private is super important. This information is really personal, so we have to make sure only the right people can get to it. To do this, strong security steps like making data unreadable (encryption) and controlling who can see what (access controls) are a must-have. Also, following rules about protecting patient info is key—like the Health Insurance Portability and Accountability Act (HIPAA) in the United States. Healthcare places and companies that make AI need to work closely together. They should share data safely and stick to strict privacy rules. By putting data privacy and security first, patients can feel good about using AI technologies for their chronic pain management in the United States.
Bridging the gap between AI potential and clinical practice
AI could really change the game for managing long-term pain, but there’s a big step to take from what it can do to actually using it in doctor’s offices. For this tech to work well, doctors and nurses need to know how they can use AI tools and understand the info these tools give them. To get there, we should set up training programs so healthcare workers get the hang of AI stuff and make smart choices when treating patients with it. By working together with experts in AI, healthcare folks can help create solutions that fit right into their day-to-day tasks without causing any hiccups. With everyone on board and informed, we’ll be able to unlock all that AI has to offer for people dealing with chronic pain.
The Future of AI in Managing Chronic Pain
The future looks bright for using AI to handle long-term pain. By looking at big sets of data, predictive analytics can figure out patterns and guess how different treatments will work on individuals. With the help of smart gadgets and sensors that you wear, ai systems can keep an eye on how much pain someone is feeling, their physical activity, and other important info as it happens. This information lets us give personalized advice right when it’s needed most to better manage pain. Thanks to predictive analytics and wearable tech working together with AI systems, we’re moving towards a big change in managing chronic pain which could really make life better for people dealing with it every day.
Predictive analytics for personalized treatment plans
With the help of machine learning and AI systems, there’s a big chance to make treatment plans that really fit people who deal with chronic pain all the time. By looking into lots of data, which includes what patients say, their medical information, and how these smart computer programs learn over time, we can spot trends and guess how different treatments might work for someone. This means doctors can come up with care plans that are just right for each person’s unique situation, making it easier to handle their pain. On top of this, predictive analytics is good at spotting things that might cause chronic pain before it even starts. So by using these advanced tools like AI and machine learning in healthcare settings helps those suffering from constant pain get better support tailored just for them.
Integrating AI with wearable technology
Combining AI with wearable tech opens up new ways to handle chronic pain. With gadgets like smartwatches or sensors, we can track how much pain someone’s feeling, how active they are, their sleep habits, and more in real time. By using AI to look at this info, it can give advice that’s tailored just for them on how to manage their pain better. For instance, based on the levels of activity and patterns of pain a person has, AI might suggest changing up daily activities or trying out certain exercises or ways to relax. This mix of wearable technology and AI could really help people dealing with chronic pain take control and make their lives better.
Patient-Centered AI Approaches
To really make a difference in managing long-term pain, it’s crucial to put the focus on what patients need and want. With AI systems, we can do just that by creating care plans tailored specifically for each person. This way, folks dealing with chronic pain can get more involved in their treatment, receiving updates and support when they need it most. On top of this, AI helps keep a steady conversation going between patients and their doctors. This means treatments can be tweaked as needed based on real-time feedback. By keeping the patient at the heart of everything, using ai systems leads to better results all around – making care more effective and centered around those who matter most.
Enhancing patient engagement through AI
AI can really help out with managing chronic pain by making it easier for patients to stay involved. With the use of AI systems, doctors and other healthcare workers can offer care that’s tailored just right and comes at the perfect time, which makes treatment work better and keeps patients happier. Through things like chatbots or virtual helpers powered by AI, people can get answers, find resources, or have someone to talk to right away without always having to go see their doctor in person. Plus, AI has this cool ability to look through stuff patients record themselves – like how they’re feeling each day or what activities they’ve been doing – so it can give advice that’s really meant just for them. By giving patients these tools driven by AI technology, they play a bigger role in handling their pain effectively which means sticking closer to their treatment plans and seeing better results overall.
Feedback loops between patients and AI systems
For managing chronic pain better, it’s really important to have a good back-and-forth between patients and AI systems. By always gathering data that patients provide and looking into it closely, AI can offer help right when it’s needed. For instance, things you wear like fitness trackers can keep an eye on how much pain you’re feeling, how active you are, and your sleep habits. Then, AI takes this info to figure out what might be causing more pain or what makes it better. This helps in giving advice that’s just for you. On top of this, these feedback loops let doctors keep track of how well treatments are working so they can make changes if needed quickly and see which methods work best. When patients work together with AI systems through these loops, dealing with chronic pain becomes a team effort which leads to getting better results for the patient.
Regulatory Landscape for AI in Healthcare
In the world of healthcare, rules about AI are changing to make sure patients stay safe and their private info is kept secret. Right now, there are some rules like HIPAA in the United States that say how patient data can be collected, stored, and used. These rules help keep patient information safe and secure. But as AI gets better and does more things in healthcare, we’re starting to see new rules made just for AI use. Looking ahead, it’s likely that these new guidelines will focus on making algorithms clear to understand while also tackling issues like bias prevention and thinking carefully about how using AI affects patient care.
Current regulations and standards
In the United States, rules and standards are super important for making sure AI is used safely and ethically in healthcare. The Health Insurance Portability and Accountability Act (HIPAA) lays down the law on how patient data should be handled – it’s all about keeping patient information private and secure. These rules require that certain steps are taken to protect this info. On top of that, groups like the Food and Drug Administration (FDA) keep an eye on AI medical devices and apps to make sure they’re up to snuff. For those working with healthcare organizations or providing AI tech, sticking to these guidelines is key for using AI responsibly, especially when it comes to managing chronic pain or other health issues.
Future directions for policy and compliance
With AI getting better and faster in the healthcare world, there’s a big need to think about what rules and guidelines we should follow. As these AI technologies keep changing, new kinds of rules that focus just on how we use AI in healthcare are starting to pop up. Looking ahead, there are a few important things these future guidelines will probably cover.
For starters, it’ll be really important for everyone to clearly see and understand how these algorithms work when they’re used for taking care of patients. Making everything more open will help doctors and their patients get why an algorithm suggests one thing over another. Then, there’s the issue of making sure no one is left out because of unfair biases hidden within these algorithms; so figuring out ways to stop this bias is key if we want everyone to get fair treatment.
Lastly, keeping an eye on ai systems regularly will make sure they stay in line with any new rules or standards as they come along. By tackling these issues head-on now,the health sector can really make the most outof using ai while also keeping patient safetyand privacy at the forefront.
Conclusion
In the world of healthcare, AI is changing how we handle chronic pain by creating tailored treatment plans and making it easier for patients to get involved. With AI getting better over time, it’s leading to smarter predictions and working smoothly with wearable tech. But, we’ve got to keep a close eye on ethics and keeping information safe so that AI can really make a difference in clinical settings. Looking ahead, there’s a lot of hope for using AI to improve care for chronic pain through exact treatments and virtual reality tools. By focusing on what patients need from AI technology, we’re looking at improving life quality for those dealing with chronic pain.
Frequently Asked Questions
How can AI improve the quality of life for chronic pain sufferers?
AI has the power to make life better for people who constantly deal with pain by creating treatment plans just for them, thanks to predictive analytics. With the help of analyzing big amounts of data and what patients share about their experiences, AI systems can spot trends and suggest specific ways to manage pain more successfully.
What are the limitations of AI in chronic pain management?
When it comes to managing chronic pain with AI systems, there are a few hurdles we can’t ignore. For starters, chronic pain is complex and how people feel pain varies from one person to another. This makes it tough for AI algorithms to always get it right when figuring out how much pain someone is in or the specific details of what they’re going through. On top of that, there are ethical issues we need to think about. These include making sure the AI doesn’t have any built-in biases and ensuring patients know what’s happening every step of the way (that’s informed consent). Another big deal is keeping patient information private since these ai systems need access to personal health data.
Key Highlights
- In the healthcare world, artificial intelligence (AI) is making big changes, especially when it comes to managing long-term pain.
- With AI tools like predictive diagnostics, natural language processing, and robotics, doctors are getting better at figuring out how to deal with pain.
- Thanks to AI, there’s a chance for more accurate diagnoses. It also helps in keeping patients involved and tailoring treatments just for them.
- There have been real examples where AI made things better in targeted medicine and even using virtual reality to help control pain.
- By bringing AI into health tech more broadly. we’re looking at a future where dealing with chronic pain could get a lot easier.