Telehealth, once a niche segment of healthcare, has become a cornerstone of modern medical care, especially after the COVID-19 pandemic accelerated its adoption. It has reshaped the way healthcare is delivered by providing more convenient, accessible, and cost-effective care. But as we look ahead to the next decade, telehealth is poised for even greater transformation. This blog explores the trends, technologies, and predictions that will shape the future of telehealth, along with key industry statistics in the U.S.
The Rise of Telehealth: A Snapshot of Today
Before diving into future predictions, it’s important to understand the current state of telehealth. The rapid adoption of telehealth services during the pandemic caused a significant shift in healthcare delivery models. According to a report from McKinsey, telehealth utilization was 78 times higher in April 2020 than it was in February 2020. While utilization rates have since stabilized, telehealth still plays a crucial role in modern healthcare.
In the U.S. alone:
- 36% of U.S. adults reported using telehealth in 2021, according to the CDC.
- 95% of large U.S. employers reported that they offered telehealth services to employees in 2021.
- Telehealth services are expected to generate $185.6 billion by 2026, as per Global Market Insights.
With its widespread acceptance, telehealth is no longer seen as a temporary solution but a vital component of healthcare. As we look ahead, several trends and emerging technologies will define its future.
Key Trends Shaping the Future of Telehealth
1. 5G Technology and Enhanced Connectivity
The rollout of 5G technology will have a significant impact on telehealth services. 5G networks offer faster, more reliable internet connections, which will improve the quality of virtual consultations, especially in rural or underserved areas with historically poor connectivity.
The low latency and high speed of 5G will also support advanced telehealth applications such as remote surgeries using robotics, real-time remote patient monitoring, and more interactive virtual care experiences. Wearable devices and IoT-enabled health monitoring tools will also benefit from 5G, as they will be able to transmit data to healthcare providers in real-time, enabling faster responses to patient health events.
By 2030, the combination of telehealth and 5G could become a lifeline for patients in remote areas, where access to high-quality healthcare has traditionally been limited.
2. Integration of Wearables and Remote Patient Monitoring
Wearable devices have already gained popularity for tracking fitness and health metrics like heart rate, steps, and sleep patterns. In the next decade, the use of remote patient monitoring (RPM) will expand dramatically as wearables become more advanced, capable of monitoring chronic conditions like diabetes, hypertension, and heart disease.
By 2030, telehealth platforms will seamlessly integrate with RPM tools to provide continuous monitoring and real-time feedback to both patients and healthcare providers. This will shift the healthcare model from reactive to proactive, enabling early intervention for potential health issues. According to a 2021 study by Insider Intelligence, 30 million U.S. patients are expected to use remote patient monitoring tools by 2024, up from 23.4 million in 2020.
The ability to monitor patients remotely will be especially beneficial for managing chronic diseases, reducing hospital admissions, and improving overall patient outcomes.
3. Telehealth and Behavioral Health Integration
Mental health is an area where telehealth has already made a profound impact. The demand for behavioral health services surged during the pandemic, with a growing number of patients seeking virtual therapy and counseling sessions. This trend is likely to continue, with telehealth becoming a key player in addressing the U.S. mental health crisis.
According to the American Psychological Association, 40% of psychologists reported that they were providing telehealth services in 2021, compared to just 7% before the pandemic. This shift has increased access to care, particularly for those in rural or underserved areas, and it has reduced the stigma associated with seeking mental health support.
Over the next decade, telehealth will integrate further into behavioral health care, offering more sophisticated virtual platforms for therapy, support groups, and mental health assessments. Digital behavioral health solutions, powered by AI and data analytics, will enable providers to monitor patients’ mental well-being more effectively and intervene early when needed.
4. Expansion of Virtual Primary Care
As telehealth continues to mature, virtual primary care services will become the norm. Many healthcare systems are already offering virtual primary care as a way for patients to regularly consult with a physician, manage chronic conditions, and get preventive care without needing to visit a clinic.
Over the next decade, this model will expand as more healthcare providers establish long-term relationships with patients through virtual means. Virtual care platforms will also offer increased access to specialist consultations, lab testing, and even virtual diagnostic services, creating a comprehensive digital healthcare ecosystem.
This shift to virtual primary care will help reduce healthcare costs, improve patient engagement, and make routine care more accessible for individuals who may otherwise avoid or delay in-person visits.
5. Regulatory and Reimbursement Changes
The rapid adoption of telehealth during the pandemic was supported by temporary regulatory changes that expanded access to telehealth services and increased reimbursement for virtual visits. As we move forward, a key factor that will shape the future of telehealth is whether these changes will become permanent.
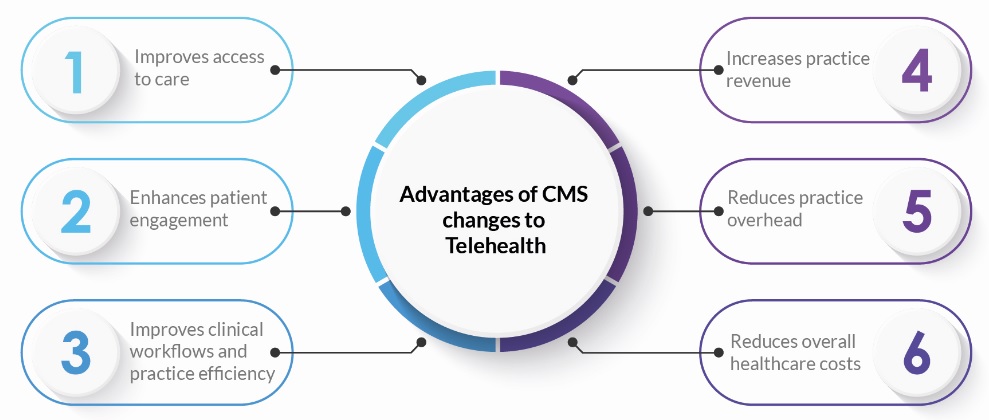
According to the Centers for Medicare & Medicaid Services (CMS), telehealth visits increased 63-fold in 2020 for Medicare beneficiaries. As of 2023, there has been growing support for making these regulatory changes permanent. Over the next decade, we can expect:
- Greater parity between telehealth and in-person reimbursement, ensuring healthcare providers are compensated fairly for virtual services.
- Expansion of cross-state licensure for healthcare providers, enabling more flexibility for patients to receive care from specialists outside their state.
- Continued government and private-sector support for broadband expansion to close the digital divide and ensure equal access to telehealth services.
6. Rise of Virtual Hospitals and Home Health
With advancements in telehealth technology, the idea of “virtual hospitals” could become a reality. Virtual hospitals will leverage telehealth platforms, RPM tools, and AI to monitor patients remotely and manage their care in real-time, reducing the need for prolonged hospital stays. This shift will also lead to more hospital-at-home programs, where patients can receive acute care services in the comfort of their homes, supported by telehealth and mobile medical technologies.
In 2021, Mayo Clinic launched a virtual hospital model, providing acute care services remotely to patients with conditions like heart failure and pneumonia. This model is expected to grow, offering a cost-effective and patient-centered approach to care. The next decade will see more healthcare systems adopt similar models, reshaping how hospital care is delivered.
7. Artificial Intelligence and Machine Learning in Telehealth
Artificial intelligence (AI) and machine learning (ML) will be at the forefront of telehealth innovations. AI-driven tools have the potential to enhance diagnostic capabilities, automate routine administrative tasks, and deliver personalized care to patients.
For instance, AI can analyze large datasets of patient information to predict potential health issues, recommend personalized treatment plans, or even detect anomalies in imaging. AI-powered chatbots and virtual assistants are already being used to provide preliminary diagnoses, saving time for both patients and healthcare providers.
By integrating AI into telehealth platforms, healthcare providers will be able to offer more accurate, efficient, and scalable services. Over the next decade, expect AI to play a larger role in both clinical decision-making and patient engagement.
Industry Statistics: Telehealth in the U.S.
- 83% of patients expect to use telemedicine after the pandemic, according to a 2021 survey by Accenture.
- The telehealth market in the U.S. is projected to grow to $307 billion by 2030, driven by increasing demand for virtual care and technological advancements.
- 63% of Medicare beneficiaries used telehealth in 2020, a dramatic increase from less than 1% in 2019.
Telehealth services saved an estimated $4 billion in healthcare costs in 2020, according to a report by McKinsey.
How HealthViewX is Shaping the Future of Telehealth
As telehealth evolves over the next decade, healthcare providers will need the right tools to meet the demands of this rapidly changing landscape. HealthViewX is at the forefront of telehealth innovation, providing a comprehensive digital health platform that enables providers to deliver high-quality virtual care.
With HealthViewX, healthcare organizations can leverage features like:
- Remote Patient Monitoring (RPM) to manage chronic conditions and improve patient outcomes.
- Telehealth integration to connect patients with their care teams, regardless of location.
- Data analytics and AI to enhance clinical decision-making and optimize care delivery.
By partnering with HealthViewX, providers can stay ahead of the curve and offer seamless, integrated telehealth services that will define the future of healthcare.
Conclusion
The future of telehealth is bright, with emerging technologies and evolving trends set to reshape the healthcare industry over the next decade. From AI-driven care to virtual hospitals, telehealth will continue to expand access, improve patient outcomes, and reduce costs. As healthcare organizations adapt to this new reality, partnering with platforms like HealthViewX will be critical to delivering the next generation of virtual care.