During the COVID-19 pandemic, CMS has taken the necessary steps to make it easier to provide quality care through telehealth services. This unprecedented action by CMS has encouraged healthcare providers to adopt and use telehealth as a way to safely provide care to their patients in situations like medication consultation, eye exams, nutrition counseling, behavioral health counseling, and routine health check-ups like annual wellness visits. Past data have shown telehealth to be an effective medium for patients to access healthcare providers especially for managing chronic conditions like diabetes, asthma or to obtain mental health counseling.
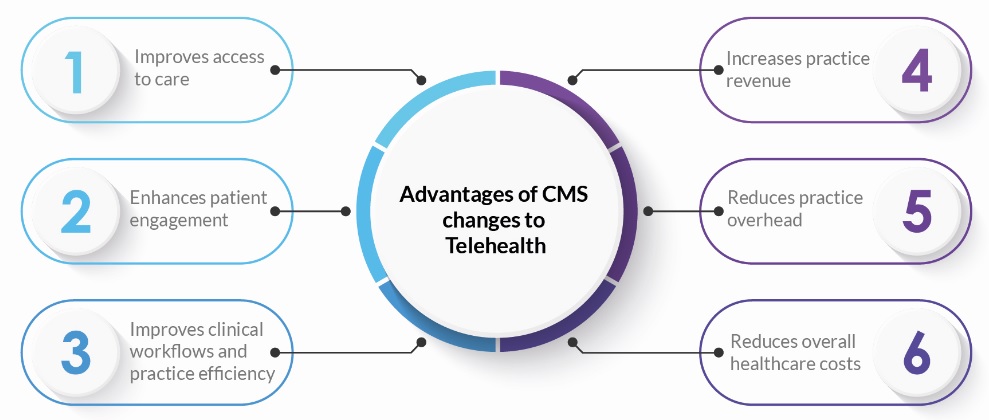
Advantages of CMS changes to Telehealth:
Telehealth services made permanent post-COVID-19:
CMS has announced that 60 of the 144 telehealth services that were newly offered during the pandemic will become permanent. This includes services for cognitive assessment, psychological and neuropsychological testing, and custodial care services for established patients.
They have also finalized the decision that direct supervision in telehealth visits can be provided with interactive audio and video technology through the end of the year until December 2021.
CPT Code |
Services |
Description |
|
77427 |
Radiation management |
It is reported once for every five fractions or treatment sessions regardless of the actual time period in which the services are furnished. The services need not be furnished on consecutive days. |
|
90853 |
Group psychotherapy |
Group psychotherapy including interpersonal interactions and support with several patients; typically 45 to 60 minutes in length. |
|
90953 |
End-stage renal disease, one visit per month, ages 2 and younger |
End-stage renal disease (ESRD) related services monthly, for patients younger than 2 years of age to include monitoring for the adequacy of nutrition, etc. |
|
90959 |
End-stage renal disease, one visit per month, ages 12-19 |
End-stage renal disease (ESRD) related services monthly, for patients 12-19 years of age to include monitoring for the adequacy of nutrition, assessment of growth |
|
90962 |
End-stage renal disease, one visit per month, ages 20 and older |
With 1 face-to-face physician visit per month |
|
92057 |
Speech/hearing therapy |
Treatment of speech, language, voice, communication, and/or auditory processing disorder, individual |
|
92521 |
Evaluation of speech fluency |
Evaluation of speech fluency (e.g., stuttering, cluttering) |
|
92522 |
Evaluation speech production |
Evaluation of speech sound production (e.g., articulation, phonological process, apraxia, dysarthria) |
|
92523 |
Speech sound language comprehension |
Evaluation of speech sound production (e.g., articulation, phonological process, apraxia, dysarthria) |
|
92524 |
Behavioral quality voice analysis |
Behavioral and qualitative analysis of voice and resonance. |
|
96130 |
Psychological test Evaluation Phys/qhp 1st |
Psychological testing evaluation services by a physician or other qualified healthcare professional, including the integration of patient data, interpretation of standardized test results and clinical data |
|
96131 |
Psychological test evaluation phys/qhp ea |
Providers should now use CPT code 96130 to bill for the first hour of psychological testing evaluation services and 96131 for each additional hour |
|
96132 |
Neuropsychological testing evaluation phys/qhp 1st |
Neuropsychological testing evaluation services by physician or other qualified healthcare professional, including integration of patient data, interpretation of standardized test results and clinical data, clinical decision making, treatment planning and report, and interactive feedback to the patient, family member(s) or caregiver(s), when performed; first hour |
|
96133 |
Neuropsychological testing evaluation phys/qhp ea |
The first hour of neuropsychological evaluation is billed using 96132 and each additional hour needed to complete the service is billed with code 96133 |
|
96136 |
Psychological and neurological testing phy/qhp 1s |
Psychological or neuropsychological test administration/scoring by physician or other qualified healthcare professional, two or more tests, any method; first 30 minutes |
|
96137 |
Psychological and neurological testing phy/qhp ea |
Similar to 96136. This code is used for each additional hour. |
|
96138 |
Psychological and neurological tech phy/qhp ea |
Psychological or neuropsychological test administration/scoring by technician, two or more tests, any method; first 30 minutes |
|
96139 |
Psychological and neurological testing tech ea |
Similar to 96138. |
|
97110 |
Therapeutic exercises |
Foundational, occupational therapy exercises that are designed to improve a patient’s strength, range of motion, endurance, or flexibility. |
|
97112 |
Neuromuscular re-education |
Specific exercises or activities performed and for what purpose, neuromuscular reeducation of movement, balance, coordination, kinesthetic sense, and/or posture. |
|
97116 |
Gait training therapy |
Therapeutic procedure, one or more areas, each 15 minutes; gait training (includes stair climbing). |
|
97161 |
Physical therapy evaluation |
Physical therapy evaluation of low complexity, 20 min |
|
97162 |
Physical therapy evaluation |
Physical therapy evaluation moderate complexity, 30 min |
|
97163 |
Physical therapy evaluation |
Physical therapy evaluation moderate complexity, 30 min |
|
97164 |
Physical therapy evaluation |
Physical therapy re-evaluation establish plan care |
|
97165 |
Occupational therapy evaluation |
Occupational therapy evaluation low complexity, 30 min |
|
97166 |
Occupational therapy evaluation |
Occupational therapy evaluation moderate complexity, 45 min |
|
97167 |
Occupational therapy evaluation |
Occupational therapy evaluation high complexity, 60 min |
|
97168 |
Occupational therapy |
Occupational therapy re-evaluation establish plan care |
|
97535 |
Self-care management training |
Direct one-on-one supervision and instruction regarding activities of daily living related to the patient’s health and hygiene. |
|
97750 |
Physical performance test |
Physical performance test or measurement (e.g., musculoskeletal, functional capacity), with written report, each 15 minutes. |
|
97755 |
Assistive technology assessment |
This procedure is used by the provider to assess the suitability and benefits of technological interfaces that will help restore, augment, or compensate for existing functional ability in the patient. |
|
97760 |
Orthotic management and training 1st en |
Orthotic(s) management and training (including assessment and fitting when not otherwise reported), upper extremity(ies), lower extremity(ies) and/or trunk, initial orthotic(s) encounter, each 15 minutes. |
|
97761 |
Prosthetic training 1st enc |
Prosthetic training, upper and/or lower extremities, initial prosthetic encounter, each 15 minutes |
|
99217 |
Observation care discharge |
This code is used to report all services provided to a patient discharged from outpatient hospital “observation status” if the discharge is on a date other than the initial date of “observation status |
|
99218 |
Initial observation care |
The first visit of the patient’s admission for outpatient hospital observation care by the Admitting/Supervising Physician or Other Qualified Healthcare Professional. Typically, 30 minutes are spent at the bedside and on the patient’s hospital floor or unit. |
|
99219 |
Initial observation care |
Similar to 99218 but, 50 minutes are spent at the bedside and on the patient’s hospital floor or unit. |
|
99220 |
Initial observation care |
Similar to 99218 but, 70 minutes are spent at the bedside and on the patient’s hospital floor or unit. |
|
99221 |
Initial hospital care |
Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician. |
|
99222 |
Initial hospital care |
Similar to 99221 |
|
99223 |
Initial hospital care |
Similar to 99221 |
|
99234 |
Observation/hospital same date |
Observation or inpatient care, are used when the patient is placed in observation status or admitted to inpatient status and then discharged on the same date. |
|
99235 |
Observation/hospital same date |
Observation or inpatient care is used when the patient is placed in observation status or admitted to inpatient status and then discharged on the same date. |
|
99236 |
Observation/hospital same date |
Observation or inpatient care is used when the patient is placed in observation status or admitted to inpatient status and then discharged on the same date. |
|
99238 |
Hospital discharge day |
Used when time spent is less than 30 minutes on the discharge process in face-to-face evaluation. |
|
99239 |
Hospital discharge day |
Used when time spent is greater than 30 minutes on the discharge process in face-to-face evaluation. |
|
99281 |
Emergency department visit |
Requires these 3 key components: A problem-focused history; A problem-focused examination; and Straightforward medical decision-making. Usually, the presenting problem(s) are self-limited or minor. |
|
99282 |
Emergency department visit |
Requires these 3 key components: An expanded problem-focused history; An expanded problem-focused examination; and Medical decision-making of low complexity. Usually, the presenting problem(s) are of low to moderate severity. |
|
99283 |
Emergency department visit |
Requires these 3 key components: An expanded problem-focused history; An expanded problem-focused examination; and Medical decision-making of moderate complexity. Usually, the presenting problem(s) are of moderate severity. |
|
99284 |
Emergency department visit |
Requires these 3 key components: A detailed history; A detailed examination; and Medical decision-making of moderate complexity. Usually, the presenting problem(s) are of high severity, and require urgent evaluation by the physician but do not pose an immediate significant threat to life or physiologic function. |
|
99285 |
Emergency department visit |
Usually, the presenting problem(s) are of high severity, and require urgent evaluation by the physician but do not pose an immediate significant threat to life or physiologic function. |
|
99291 |
Critical care first hour |
It is used to report the services of a physician providing full attention to a critically ill or critically injured patient from 30-74 minutes on a given date |
|
99292 |
Critical care additional 30 mins |
Code 99292 (critical care, each additional 30 minutes) is used to report additional block(s) of time, of up to 30 minutes each beyond the first 74 minutes of critical care. |
|
99304 |
Nursing facility care initial |
The problem(s) requiring admission are of low severity. Typically, 25 minutes are spent at the bedside and on the patient’s facility floor or unit. |
|
99305 |
Nursing facility care initial |
The problem(s) requiring admission are of moderate severity. Typically, 35 minutes are spent at the bedside and on the patient’s facility floor or unit. |
|
99306 |
Nursing facility care initial |
The problem(s) requiring admission are of high severity. Typically, 45 minutes are spent at the bedside and on the patient’s facility floor or unit. |
|
99315 |
Nursing facility discharge day |
99315 is for discharge day management 30 minutes or less |
|
99316 |
Nursing facility discharge day |
This code is for discharge day management over 30 minutes |
|
99327 |
Domiciliary or rest home visit new patient |
Domiciliary or rest home visit for the evaluation and management of a new patient. Usually, the presenting problem(s) are of high severity. Typically, 60 minutes are spent face-to-face with the patient and/or family. |
|
99328 |
Domiciliary or rest home visit new patient |
Code used for Evaluation and Management / Domiciliary, rest home (boarding home) or custodial care services. The general guidance for this code is that it is used for new patient assisted living visits, typically 75 minutes. |
|
99334 |
Domiciliary or rest home visit established patient |
This code 99334 is used to reflect the domiciliary or rest home visit for the E/M of an established patient |
|
99335 |
Domiciliary or rest home visit established patient |
Similar to 99334 |
|
99336 |
Domiciliary or rest home visit established patient |
Similar to 99334 |
|
99337 |
Domiciliary or rest home visit established patient |
Domiciliary or rest home visit for the evaluation and management of an established patient. Usually, the presenting problem(s) are moderate to high severity. Typically, 60 minutes are spent face-to-face with the patient and/or family |
|
99341 |
Home visit new patient |
Home services are provided in a private residence. A home visit cannot be billed by a physician unless the physician was actually present in the beneficiary’s home. Level 1 new patient home visit. |
|
99342 |
Home visit new patient |
Home services are provided in a private residence. A home visit cannot be billed by a physician unless the physician was actually present in the beneficiary’s home. Level 2 new patient home visit. |
|
99343 |
Home visit new patient |
Home services are provided in a private residence. A home visit cannot be billed by a physician unless the physician was actually present in the beneficiary’s home. Level 3 new patient home visit. |
|
99344 |
Home visit new patient |
Home services are provided in a private residence. A home visit cannot be billed by a physician unless the physician was actually present in the beneficiary’s home. Level 4 new patient home visit. |
|
99345 |
Home visit new patient |
Home services are provided in a private residence. A home visit cannot be billed by a physician unless the physician was actually present in the beneficiary’s home.Level 5 new patient home visit. |
|
99347 |
Home visit established patient |
Home visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components. A problem-focused interval history; a problem-focused examination; and straightforward medical decision making. Typically, 15 minutes are spent face-to-face with the patient and/or family. |
|
99348 |
Home visit established patient |
Similar to CPT Code 99348. Typically, 25 minutes are spent face-to-face with the patient and/or family. |
|
99349 |
Home visit established patient |
Similar to CPT Code 99348. Typically, 40 minutes are spent face-to-face with the patient and/or family. |
|
99350 |
Home visit established patient |
Similar to CPT Code 99348. Typically, 60 minutes are spent face-to-face with the patient and/or family. |
|
99468 |
Neonatal critical care initial |
Services of directing the inpatient care of a critically ill neonate or infant 28 days or younger. |
|
99469 |
Neonatal critical care initial |
Services of directing the inpatient care of a critically ill neonate or infant 28 days or younger. |
|
99471 |
Pediatric critical care initial |
Initial inpatient pediatric critical care, per day, for the evaluation and management of a critically ill infant or young child, 29 days through 24 months of age |
|
99472 |
Pediatric critical care initial |
Subsequent inpatient pediatric critical care, per day, for the evaluation and management of a critically ill infant or young child, 29 days through 24 months of age |
|
99473 |
Self-measurement of blood pressure at home education/training |
Code 99473 represents the work of training the patient and calibrating the device, |
|
99475 |
Pediatric critical care ages 2-5 initial |
Initial inpatient pediatric critical care, per day, for the evaluation and management of a critically ill infant or young child, 2 through 5 years of age |
|
99476 |
Pediatric critical care ages 2-5 subsequent |
Subsequent inpatient pediatric critical care, per day, for the evaluation and management of a critically ill infant or young child, 2 through 5 years of age |
|
99477 |
Initial day of hospital care for neonatal care |
Initial hospital care of the neonate (28 days or younger) who is not critically ill but requires intensive observation, frequent interventions, and other intensive care services. |
|
99478 |
Ic low-birthweight infant |
Intensive care, per day, for the evaluation and management of the recovering low or very low birth weight infant( < 1500 gm) |
|
99479 |
Ic low-birthweight infant < 1500-2500 g subsequent |
Intensive care, per day, for the evaluation and management of the recovering low or very low birth weight infant( 1500 gm-2500g) |
|
99480 |
Ic infant pbw 2501-5000 g subsequent |
Intensive care, per day, for the evaluation and management of the recovering low or very low birth weight infant(2501g-5000g) |
|
99483 |
Assessment and care plan cognitive impairment |
Assessment of and care planning for a patient with cognitive impairment, requiring an independent historian, in the office or other outpatient, home or domiciliary or rest home |
The ongoing pandemic has resulted in an increased workload for healthcare providers across the country. Incorporating telehealth software into an existing practice can allow providers to virtually connect with patients. This can relieve the strain on practice while introducing an additional revenue stream.
HealthViewX Telehealth/Telemedicine Platform helps health systems to align clinical, financial, and operational goals by providing high-quality remote care and enhancing patient-physician collaborations.