As healthcare practices strive to deliver quality patient care while managing operational costs, Remote Physiologic Monitoring (RPM) has emerged as a game-changer. The Centers for Medicare & Medicaid Services (CMS) has recognized the value of RPM in chronic disease management, creating lucrative opportunities for care practices to enhance patient outcomes and boost revenue streams. In this comprehensive guide, we’ll explore how Medicare’s RPM program can drive revenue growth, outline essential billing codes and reimbursement rates, and highlight how HealthViewX can streamline the delivery of RPM services.
What is Medicare Remote Physiologic Monitoring (RPM)?
Medicare RPM is a care management program designed to monitor patients’ physiologic data remotely, enabling proactive management of chronic conditions. RPM leverages digital technologies to collect data such as heart rate, blood pressure, glucose levels, and weight from patients in their homes. This data is then transmitted to healthcare providers, allowing for timely interventions and personalized care adjustments.
Key Benefits of RPM for Care Practices:
- Improved Patient Outcomes: Early detection of health issues reduces hospitalizations and emergency room visits.
- Enhanced Patient Engagement: Regular monitoring encourages patients to take an active role in their health.
- New Revenue Stream: Care practices can generate additional income through Medicare reimbursements.
Market Insights and CMS Statistics
The demand for RPM is rapidly growing, driven by the increasing prevalence of chronic diseases and the need for value-based care. According to CMS data:
- Over 37 million Medicare beneficiaries have multiple chronic conditions, making them eligible for RPM services.
- The remote patient monitoring market in the U.S. is expected to reach $2.14 billion by 2027, growing at a CAGR of 13.5%.
These statistics highlight the significant potential for care practices to adopt RPM and leverage Medicare reimbursements to improve patient outcomes while driving revenue growth.
Medicare RPM Billing Codes and Reimbursement Rates
CMS has outlined specific CPT codes for RPM services, allowing care practices to receive reimbursements for monitoring patients remotely. Below are the essential billing codes, their descriptions, and the associated reimbursement rates for 2024:
1. CPT Code 99453
- Description: Initial set-up and patient education on the use of RPM devices.
- Reimbursement Rate: Approximately $19.32 (one-time payment per patient).
- Eligibility: This code is used to bill for the time spent setting up the device and educating the patient on its use.
2. CPT Code 99454
- Description: Supply of devices that collect and transmit data daily for at least 16 days.
- Reimbursement Rate: Approximately $48.80 per month.
- Eligibility: Covers device usage and data transmission.
3. CPT Code 99091
- Description: Collection and interpretation of physiologic data (e.g., ECG, blood pressure) that has been digitally stored and/or transmitted.
- Reimbursement Rate: Approximately $56.88 per 30-day period.
- Eligibility: Requires a minimum of 20 minutes of clinical staff time per month.
4. CPT Code 99457
- Description: Remote physiologic monitoring treatment management services, with a minimum of 20 minutes of interactive communication with the patient/caregiver during the month.
- Reimbursement Rate: Approximately $50.94 per month.
- Eligibility: Can be billed once a month per patient.
5. CPT Code 99458
- Description: Additional 20 minutes of RPM management services.
- Reimbursement Rate: Approximately $41.17 per month.
- Eligibility: This code is add-on to 99457 for extended management.
These codes collectively enable care practices to generate recurring revenue by delivering RPM services, making it a viable model for financial sustainability.
How Medicare RPM Can Boost Your Practice’s Revenue
Implementing an RPM program not only enhances patient care but also provides a substantial revenue opportunity. Here’s how:
1. Increased Reimbursement Potential
By enrolling eligible patients in RPM, care practices can significantly increase their monthly revenue. For example, billing CPT codes 99453, 99454, 99457, and 99458 for a single patient can result in over $150 per patient per month. With just 100 RPM patients, this could translate to an additional revenue stream of $15,000 per month or $180,000 annually.
2. Improved Patient Retention
RPM services enhance patient satisfaction by providing personalized, continuous care. This results in better patient retention and loyalty, ultimately increasing your practice’s patient base and revenue.
3. Cost Efficiency
RPM reduces the need for frequent in-office visits, cutting down operational costs while allowing healthcare providers to manage more patients efficiently. This scalability ensures sustainable revenue growth.
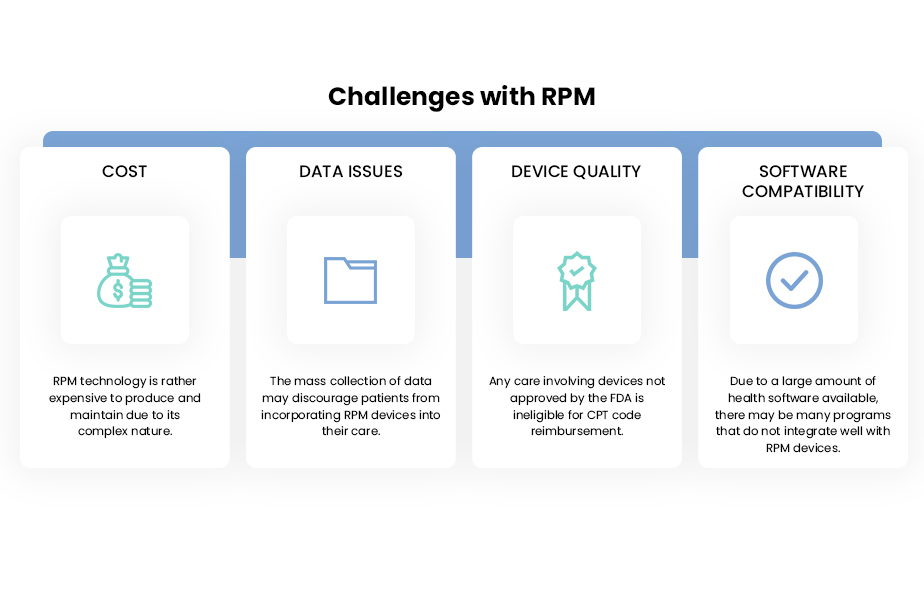
Overcoming Challenges with HealthViewX RPM Solutions
While the Medicare RPM program presents substantial financial and clinical benefits, implementing an effective RPM strategy can be challenging. This is where HealthViewX comes into play.
How HealthViewX Can Help Your Practice Deliver RPM Services
HealthViewX is a leading digital health platform that empowers care practices to efficiently deliver RPM services. Here’s how HealthViewX can support your RPM program:
1. Comprehensive RPM Platform
- Seamless Device Integration: HealthViewX supports a wide range of RPM devices, enabling real-time data capture and transmission.
- Automated Data Analytics: The platform automatically analyzes patient data, providing actionable insights for proactive patient management.
- Customizable Alerts: Set up customized alerts for critical readings to ensure timely interventions.
2. Streamlined Billing and Compliance
- Automated Billing Workflow: HealthViewX simplifies billing with automated claims submission and tracking, ensuring accurate and timely reimbursements.
- Compliance Management: The platform is fully compliant with CMS guidelines, reducing the risk of billing errors and audits.
- Real-Time Reporting: Generate detailed reports on patient interactions, billing compliance, and RPM outcomes.
3. Enhanced Patient Engagement
- User-Friendly Patient Portal: Patients can easily access their health data, engage with care teams, and track their progress.
- Remote Communication Tools: HealthViewX provides secure messaging, video consultations, and real-time alerts to enhance patient-provider communication.
4. Scalable Solution for Growth
- Scalable Architecture: Whether you have 50 or 5,000 patients, HealthViewX can scale to meet your practice’s needs.
- Dedicated Support Team: Benefit from expert support and training to ensure a smooth RPM program rollout and sustained success.
Conclusion
The Medicare Remote Physiologic Monitoring program offers a win-win opportunity for care practices to boost revenue while improving patient care. By leveraging CMS RPM billing codes and reimbursement rates, practices can unlock new revenue streams and achieve value-based care goals. Implementing a robust RPM strategy, however, requires the right tools and expertise.
HealthViewX provides a comprehensive RPM platform designed to simplify the delivery of remote monitoring services, optimize billing, and enhance patient engagement. By partnering with HealthViewX, your practice can seamlessly integrate RPM into your care model, driving better patient outcomes and maximizing revenue potential.
Ready to transform your practice with RPM? Contact HealthViewX today to schedule a demo and explore how we can support your RPM journey.